Search and destroy: Knocking
down a deadly brain cancer
Together with NUS researchers, NUH is set to start clinical trials for a promising stem-cell based therapy, potentially offering a lifeline for patients with a deadly form of brain cancer.
Issue 1 | June 2023
 Subscribe and ensure you don't miss the next issue!
Subscribe and ensure you don't miss the next issue!
Headaches, memory loss and behavioural changes—when signs of neurological impairment arise, the culprits that often come to mind are the likes of Alzheimer’s disease or traumatic brain injuries. However, these issues can also be caused by a vicious cancer called glioblastoma.
Not only is it the most common form of
brain tumour, but glioblastoma is extremely difficult to tame. Even with interventions, post-diagnosis survival only lasts for around two to three years. To make matters worse, glioblastoma has a near-100 per cent recurrence rate; patients get little reprieve as the cancer keeps coming back, each time more destructive than the last.
But not all hope is lost. A stealthy new approach involving stem cell-based gene therapy could soon revolutionise human patient outcomes for aggressive tumours.
In collaboration with the treatment’s developers from the National University of Singapore Yong Loo Lin School of Medicine (NUS Medicine), a team led by Clin Assoc Prof Yeo plans to initiate clinical trials for patients with recurrent glioblastoma, hoping to offer them a chance at a better life.
A silent killer
Glioblastomas start from the glia, which are support cells that are critical for the normal functioning of neurons—from facilitating metabolic processes to modulating their connectivity and communication. This highly aggressive cancer can rapidly grow and invade surrounding brain tissue, impeding various neural functions such as attention and sensory processing depending on the tumour’s location.
But extracting these tumours comes with its own host of complications, even when done by the best surgeons. The entirety of the cancerous mass cannot always be removed, as the surrounding brain tissue might get caught in the fray and pose a high risk of inducing long-term neurological damage.
“One of the main problems with cancer drugs is typically not the effectiveness, but more so their specificity,” explains Clin Assoc Prof Yeo. Many compounds including the chemotherapy fluorouracil (5FU) are highly toxic to cancer cells, but they can also disrupt normal cellular processes, leading to severe side effects.
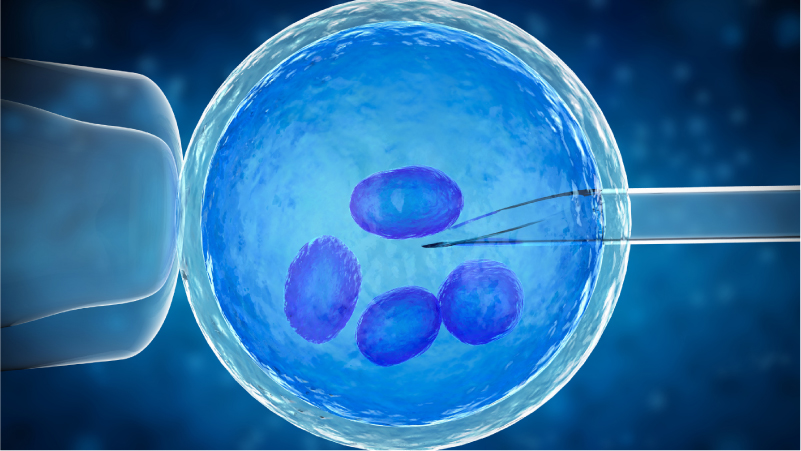
To circumvent this dilemma, the therapeutic strategy devised by NUS Medicine researchers makes use of stem cells that act like Trojan horses to deliver the 5FU therapy directly to the tumour. Stem cells are precursors to specialised cells like neurons or muscle cells, but they are still in their undifferentiated form. Accordingly, they can be engineered to transform into certain cell types or perform modified functions, opening avenues for innovative medical interventions.
The team introduced yeast genes into the stem cells, which localise to the tumour site inside the body, surrounding the cancer cells like a homing device. While the stem cells themselves are not toxic, taking in a readily available anti-fungal drug will trigger a reaction with the yeast genes, switching on their expression and leading to the transformation into the cancer-killing 5FU.
By targeting only the cancer cells, the stem cell-based therapy has a lower risk of inducing serious side effects compared to traditional 5FU. Once the cancerous mass has been cleared out, the modified stem cells themselves also die—getting the job done and leaving without a trace.
From bench to bark to bedside
Over the last few years, the novel approach has begun to make headway into real-world usage, beginning with veterinary practice. Out of over 60 dogs and cats with varying cancer types, the stem cell-based therapy had an astounding impact for 80 per cent of them—allowing the animals to either live longer than expected, or have a better quality of life with reduced suffering. Several of their tumours stayed small without regrowing, with 14 even completely disappearing for at least 30 months post-treatment.
“With such promising results, we want to harness the power of this novel therapy to hopefully change the lives of human patients as well,” shares Clin Assoc Prof Yeo.
Local clinical trials are set to begin in 2024, and should they prove successful, the modified stem cells will have to be made in bulk to meet the needs of glioblastoma patients. But Dr Sarah Ho, a senior research fellow at NUS Medicine’s Department of Biochemistry, and her team are not too worried about a production bottleneck.
Currently, an adequate stem cell supply can be produced for up to 18 patients each week. Scaling up manufacturing is also more affordable, standing at less than 10 per cent of the multi-million cost for using viral gene carriers.
The advancement of stem cell technologies is bound to transform the future of healthcare, offering renewed hope for cancer patients that may otherwise have no options left.
“Novel therapies that can selectively target tumours could be a game-changer to mitigate the devastating effects of these diseases and enhance the welfare of patients and their families,” Clin Assoc Prof Yeo concludes.
Like this article? Simply subscribe to make sure you don't miss the next issue of EnvisioningHealth!