Services for Urinary Incontinence
2024/05/15
To diagnose urinary incontinence, a series of tests will be conducted. The process entails detailed discussions about current symptoms and medical history. A physical examination is also needed, including an examination of the genitalia region. The questions asked by the urologist may include:
- Current symptoms (e.g., number of times you visit the toilet and number of leakages a day, situations when you leak urine);
- Duration of symptoms;
- List of the medications you are taking;
- Previous surgical procedures;
- Other diseases or condition;
- Bowel habits;
- Lifestyle (exercising, smoking, alcohol consumption and diet);
- Pregnancy history;
- Menstruation history and menopausal problems;
- Sexual history.
The urologist will do a general physical examination on:
- Abdomen
- Genitals (pelvic examination for females)
Grading of urinary incontinence:
Stress incontinence can be broadly categorised into three grades based on severity.
Grade 1 (mild): Leakage occurs only when there is severe abdominal straining (e.g., coughing or sneezing). There is generally no need for pads and there is no leakage during normal exercise and at night.
Grade 2 (moderate): Leakage occurs during moderate abdominal straining (e.g., running or exercise). Pads may be needed, and the number of leakages is greater than in Grade 1.
Grade 3 (severe): Leakage occurs with mild stress (e.g., standing up from a sitting position or lying down position). Pads are needed all the time due to frequent leakage episodes, becoming a social or hygiene concern.
Urine test
You will be asked to provides a urine sample for tests to exclude urinary tract infection and traces of blood in the urine.
Bladder diary
Keep a bladder diary, noting your fluid intake, urination frequency and urine volume. The diary helps your doctor understand your symptoms better. You may be asked to purchase a measurement jug if you do not have one.
Urodynamic study (UDS)
UDS is performed to gather more information about the urination process and assess the functionality of the bladder muscles. The goal is to replicate the urinary symptoms during the study. Small catheters are inserted into your urethra and rectum to measure pressure during fluid instillation into the bladder.
Uroflowmetry (selected cases)
This is a simple test which electronically records the rate of urine flow. The patient will urinate into a container known as a uroflowmeter. This test is useful in identifying potential obstructions to urine flow.
Imaging of the bladder/kidneys (selected cases)
An ultrasound of the bladder and kidneys, using high-frequency sounds to create images of the bladder/kidneys.
Cystoscopy (selected cases)
Flexible cystoscopy is performed if there is blood in the urine or abnormal ultrasound findings. It is a day procedure allowing direct visualisation of the bladder to assess for other conditions.
Stress urinary incontinence (SUI) is often bothersome but not life-threatening. Initial treatment typically involves self-management strategies. Discuss these options with your urologist and actively engage in managing your symptoms. Consider the following self-management measures:
- Fluid restriction after counselling
- If there is severe leakage, absorbent pads/adult diapers may be used
- Bladder retraining
- Avoid constipation and known triggers
- Weight loss
- Pelvic floor exercise (also known as Kegel exercises)
In cases where self-management or lifestyle changes are inadequate to control symptoms, medications may be prescribed. A common medication is local oestrogen application for postmenopausal females to improve the pelvic floor tissues.
For patients experiencing Grade 3 or severe incontinence, surgery may be offered. In general, this is considered for those who have not responded to conservative treatment or those seeking an improved quality of life. Surgery may involve lifting of the urethra or bulking up the sphincter muscle to bolster closure mechanism. Additional surgeries may be needed to correct pelvic organ prolapse.
Common surgeries for female SUI:
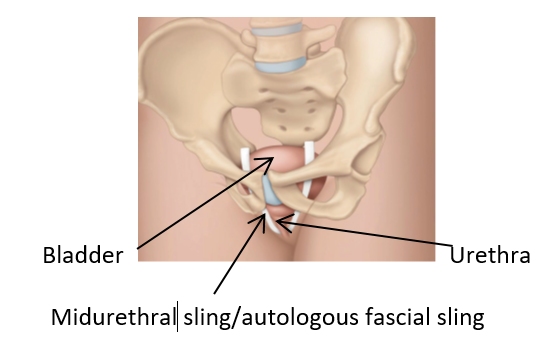
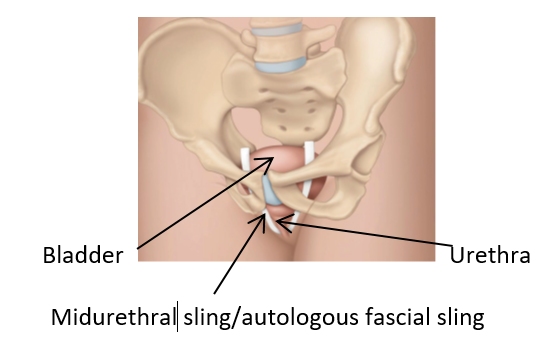
Midurethral sling (MUS): A synthetic mesh strap/ribbon placed under the urethra to provide support.
Autologous fascial sling: A strap/ribbon made from the patient's own body tissue (harvested from the abdomen or thigh) placed under the urethra to provide support.
Burch colposuspension: An operation to support the bladder neck, which connects the bladder to the urethra, to resist pressure.
Bulking agents: Injection of substance into the urethral walls to improve closure; effects are usually temporary and may need repeat procedures.

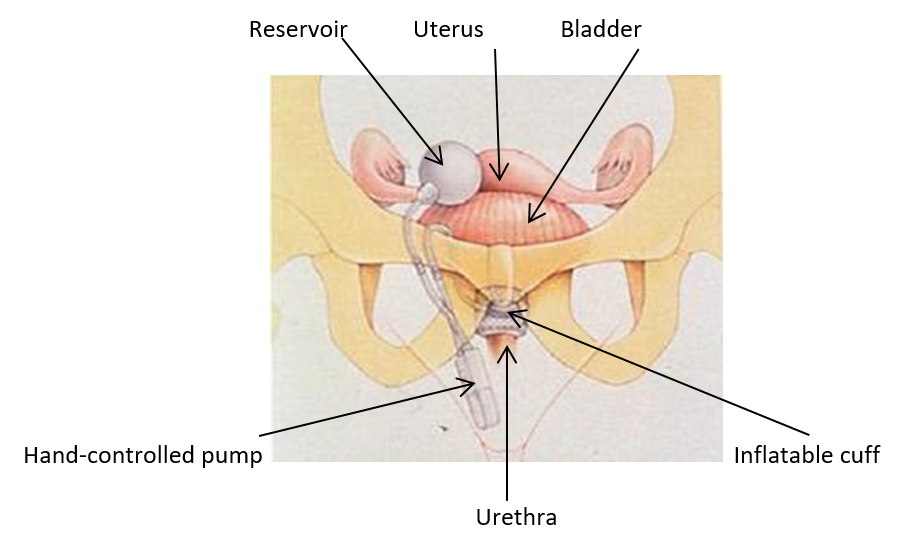
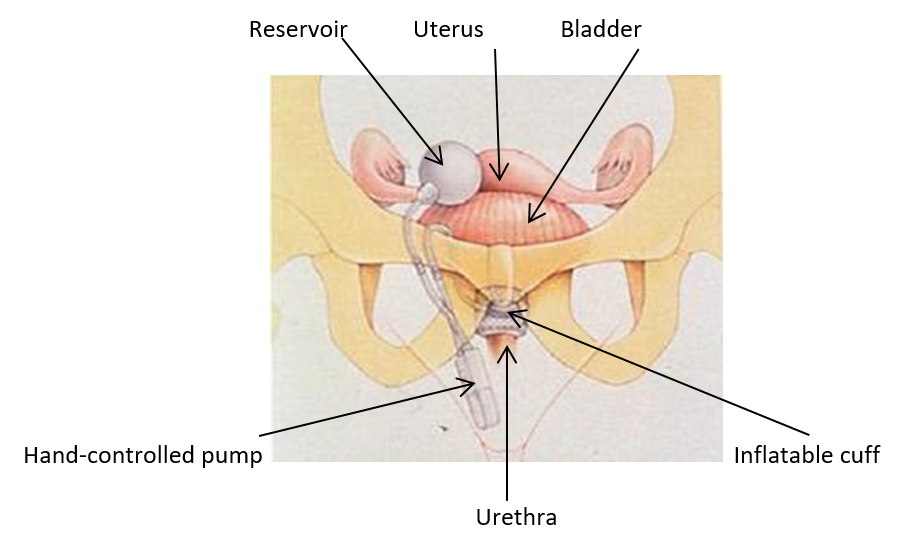
Artificial urinary sphincter (AUS): An inflatable cuff placed around the urethra connected to a hand controlled pump, allowing controlled urine release.
Please consult your doctor or nurse regarding any questions or concerns about incontinence. You should not feel embarrassed to reach out as your well-being is a top priority.