A brain aneurysm is a swollen bulge or “ballooning” in the wall of a blood vessel in the brain. An aneurysm is a very serious, life-threatening emergency that needs to be treated right away. It leads to a bleeding (haemorrhagic) stroke. A “stroke” is a term doctors use when a part of the brain is damaged because of a problem with the blood vessels in the brain.
Signs and symptoms of a brain aneurysm
Most brain aneurysms have no symptoms. But a large aneurysm can cause symptoms that include:
- Severe headache
- Pain in the face
- Blurry or double vision
If the aneurysm ruptures, symptoms can include:
- Sudden, severe headache - people may describe it as the worst headache they ever had
- Stiff neck
- Nausea and vomiting
- Double vision
- Drowsy
- Coma
Factors which may increase one’s risk of having a brain aneurysm
- Having strong family history
- High blood pressure
- Smoking
- Drinking too much alcohol
- Using illegal drugs, such as cocaine or amphetamines
- Taking diet pills
Tests to diagnose a brain aneurysm
The doctor may perform several different tests to diagnose brain aneurysm for patients who are displaying the symptoms:
- Imaging tests
CT scan and an MRI. Both show pictures of your brain. During these tests, you may be given an injection of a dye, which makes it easier for doctors to see the blood flow in the brain. - Cerebral angiogram
For this test, your doctor will insert a thin plastic tube into a large blood vessel at the groin. Then, the tube will be advanced through your blood vessels past your heart to your brain. Your doctor will then inject a dye which will show up on the x-ray. This will allow the doctor to see the blood vessels in your brain to find the aneurysm.
Treatments for brain aneurysm
The treatment of brain aneurysm is very critical, and the best option of treatment is entirely based on the patient's underlying condition, type and size of aneurysm, as well as a collaborative decision-making process between the neurosurgeon, interventional radiologist and patient.
- Surgical clipping
In this surgery, your doctor will place a tiny metal clip on the base of the aneurysm to stop the blood flow to it. - Endovascular coiling
The first part of this treatment is the same procedure as a cerebral angiogram (see above). On top of injecting dye into the tube, your doctor will insert a special soft wire through your blood vessels into the aneurysm sac. The wire will then detach tiny titanium coils inside the aneurysm sac and seal it off from the blood vessel.
How should the patient prepare for the surgery?Before surgery, preparations that need to be done include:
- Pre-operative investigations such as chest x-ray, electrocardiogram (ECG) and blood tests.
- No food and drinks for at least 12 hours.
- Decisions regarding treatment are made by the patient when capable. In cases where the patient is incapacitated, two consultants will collaboratively assess and determine the appropriate course of action. It's important to note that no written consent is required from next of kin in these situations.
What can the patient expect immediately after surgery?
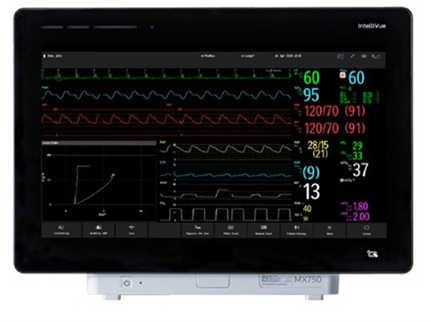
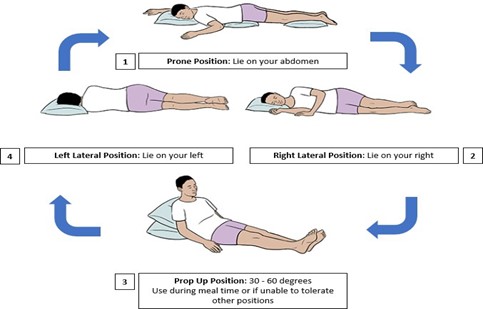
- The patient may be required to stay in ICU or HD facility for close monitoring.
- Presence of wound dressing, intravenous drip and head drain.
- Presence of urinary catheter
- Hourly monitoring of urine output
- Frequent monitoring of vital signs and head chart.
- For diet intake, there will be a gradual increase from nothing by mouth to diet of your choice.
- Patient will be given painkillers for pain relief.
- In surgical clipping, patient’s hair will be shaved off for the doctor to access the area to be operated on.
Length of hospitalisationThe length of hospitalisation for patients who have suffered subarachnoid haemorrhage is dependent on patient’s condition upon admission, and the treatment of concomitant issues such as cerebral vasospasm, hydrocephalus and respiratory issues. In patients with severe subarachnoid haemorrhage, hospitalisation may be up to three to four weeks.
Important points to note after surgery- Patient should not start doing any strenuous activities such as running, climbing, swimming until they have received clearance from their doctor to do so.
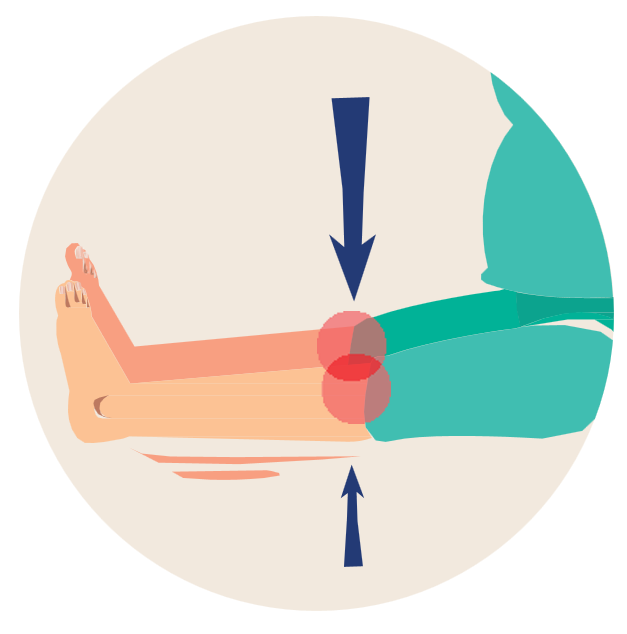
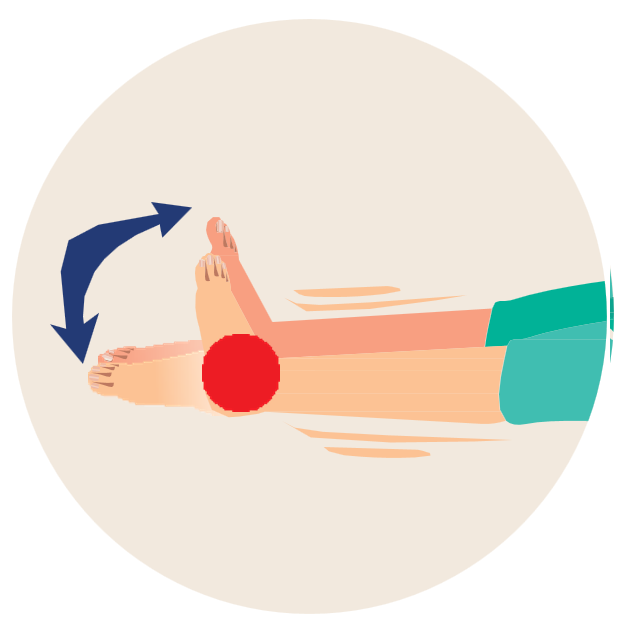
- Patient should do light exercises as taught by the physiotherapist.
- If patient is discharged with a dressing on the surgical site, they should get an outpatient appointment for removal of stitches before leaving the hospital.
- Patient should not wet the dressing during shower. If the dressing gets wet, patient can go to the nearest clinic/polyclinic to have the wound cleaned and dressed.
If the patient experiences any of the following symptoms, proceed to the NUH Emergency Department immediately:
- Signs of infection such as fever equal to or more than 38.0 degrees
- Pain at the surgical site
- Swelling, redness or leaking from the surgical site
- Headache, vomiting, weakness, seizures, blurred vision and drowsiness.