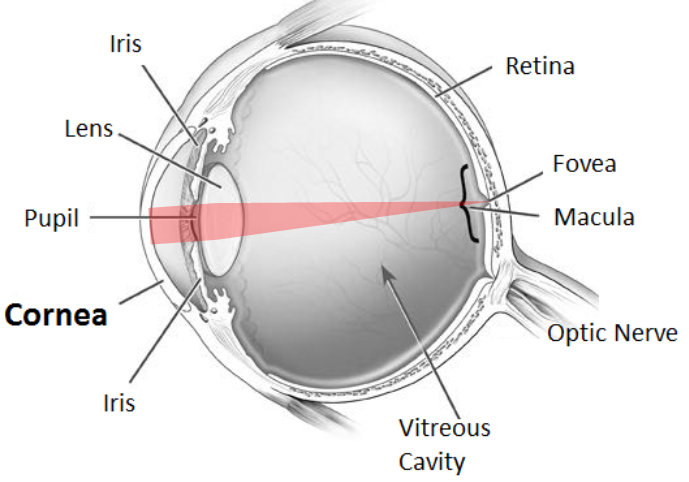
What Is the Cornea and What Is Its Function?
The cornea is the clear outermost layer of the eye. It plays an important role in providing clear vision by refracting incoming light onto the lens, which is then refocused onto the retina, an area where conversion of light into vision occurs.
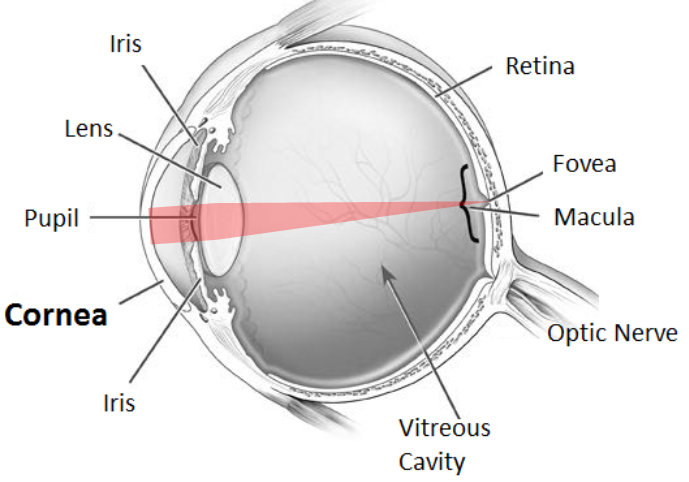
A diseased cornea prevents light rays from reaching the retina, resulting in poor vision. In some cases, a corneal transplant may be necessary to restore visual function.
What Is a Corneal Transplant?
Corneal transplant surgery involves the removal of the damaged cornea and replacing it with a healthy donor cornea.
What Are the Different Types of Corneal Transplant?
There are two main types of corneal transplants:
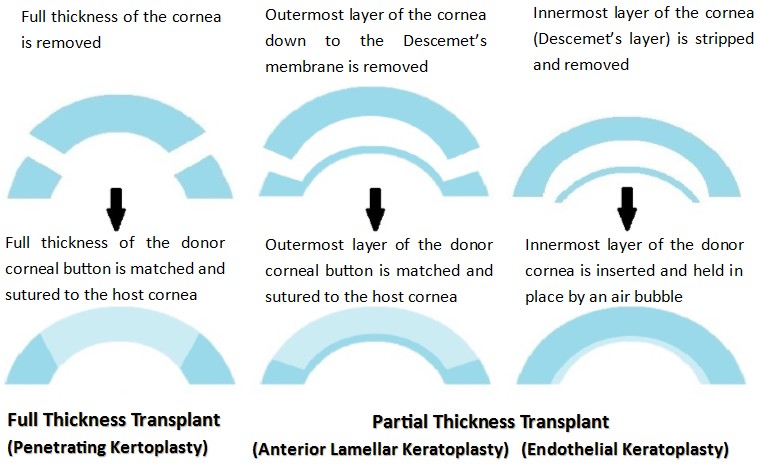
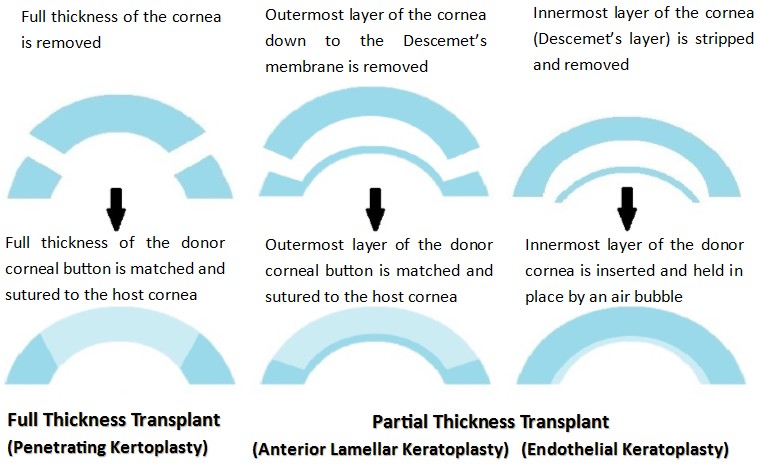
Full thickness corneal transplant (Penetrating Keratoplasty), which involves the complete replacement of the cornea.
Partial thickness corneal transplant, which includes either transplanting the outer layer of the cornea (Anterior Lamellar Keratoplasty) or the innermost layer (Endothelial Keratoplasty).
The corneal specialist will advise on the appropriate surgery according the individual's specific needs.
Why the National University Hospital?
The NUH paediatric Corneal Transplant Team is made up of corneal specialists, paediatric ophthalmologists, glaucomatologists, optometrists, the paediatric transplant team and anaesthetists. This multi-disciplinary approach to care is especially important in paediatric cases with a high risk of rejection and graft failure. We offer comprehensive pre- and post-transplant evaluation, including individualised peri-operative immunosuppression and post-operative visual rehabilitation to prevent graft rejection, thereby optimising visual outcome.
Who Will Need a Corneal Transplant?
Corneal transplants can be used to treat both congenital and acquired corneal diseases. Common congenital causes of corneal opacities/oedema include congenital hereditary endothelial dystrophy, posterior polymorphous corneal dystrophy, congenital hereditary stromal dystrophy, Peters' anomaly, congenital glaucoma, sclero-cornea, epibulbardermoid and metabolic disorders. Common acquired causes of corneal opacities/oedema include trauma-related corneal injuries, corneal scars, keratoconus, keratoglobus, Stevens-Johnson syndrome and toxic epidermal necrolysis.
How Is a Corneal Transplant Performed?
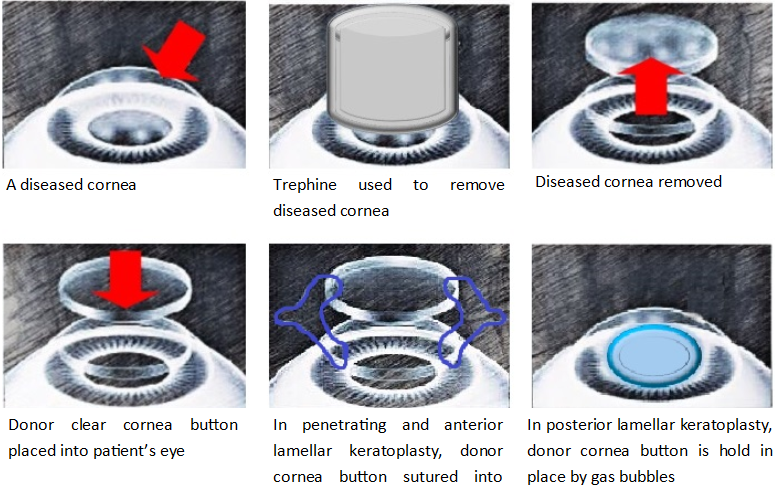
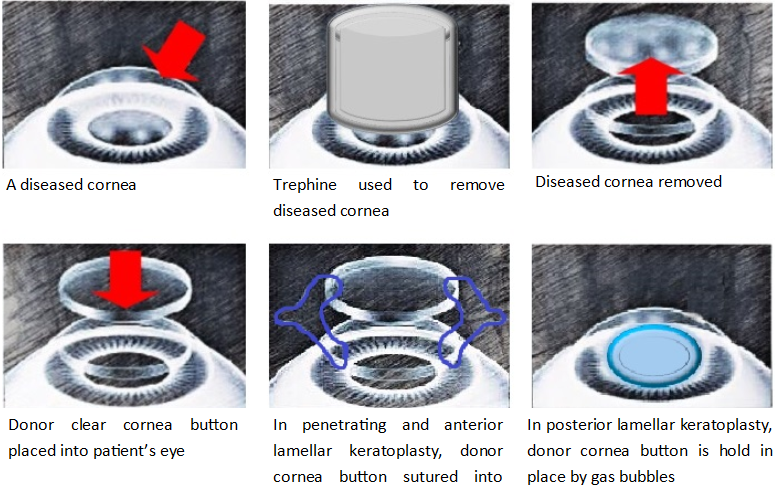
Performed under general anesthesia, the corneal transplant involves removing the diseased cornea and replacing it with a clear donor cornea button, securely fastened with sutures.
In Endothelial Keratoplasty, a gas bubble is injected into the eye to tamponade the transplanted graft in place. Maintaining a post-operative supine position for 1-2 days is crucial in these cases.
The surgery is usually performed as a day surgery procedure. Admission and assessment by a pre-operative anaesthetist may be required for high-risk patients
What Is the Success Rate of Corneal Transplant?
The success rate for corneal transplants exceeds 90%. Although patients may experience astigmatism, leading to some degree of visual blurring, the majority witness significant improvement in vision over the initial months post-transplant.
What Are the Risks of a Corneal Transplant?
Risks of corneal transplants include, but are not limited to ocular bleeding, infection such as keratitis or endophthalmitis, glaucoma, graft rejection, cataract formation and retinal detachment. The operative risks include those of general anaesthesia.
What Is Corneal Graft Rejection and How Is It Treated?
Graft rejection is a recognized complication wherein the immune system perceives the donor cornea as foreign and attacks it. While rejection can occur at any time post-transplant, it is most common within the first two years. Approximately 20% of corneal transplants face rejection, typically treatable with immunosuppressive therapy. Repeat transplants carry a higher risk, necessitating more intensive immunosuppressive measures.
What Is the Care Required After Corneal Transplant?
Frequent administration of topical steroid eyedrops for at least fiveyears (depending on the type of transplant) after corneal transplant is essential to reduce the risk of graft rejection. Administering eyedrops to infants or young children may pose challenges, requiring patience and diligence from caregivers.
For infants and young children unable to cooperate with post-operative examination, sedation or anaesthesia may be required after a corneal transplant. Suture removal is usually performed a few months to years later, depending on the rate of recovery, presence of suture-related complications, and the degree of induced-astigmatism.
What Is the Long-Term Care After a Corneal Transplant?
After a corneal transplant, the focus shifts to long-term care, particularly in the case of infants and children undergoing keratoplasty. Successful visual rehabilitation requires addressing factors like amblyopia ('lazy eye') resulting from pre-surgery visual deprivation, graft astigmatism, and anisometropia. Collaborative care with a Paediatric Ophthalmologist is crucial for optimising post-operative visual recovery.
What Can You Do as the Caregiver at Home?
Children tend to rub their eyes during the healing period, risking broken sutures and corneal wound dehiscence. These actions may increase the risk of rejection and infection. Caregivers should observe for increased eye redness, corneal haziness or opacities. Any reported drop in vision or pain requires prompt attention, necessitating an early appointment to address concerns promptly.
Where Can I Find out More Information?
Book an appointment with the NUH Eye Surgery Centre for a comprehensive eye check-up and recommendations for your individualised treatment plan.